Introduction
There was an unusual sense of solidarity in the world during the first few months after the COVID-19 virus was first discovered. An acknowledgement that we were all going through the same struggles: lockdowns, restrictions, hospitals at capacity and the need for contingency plans. The pandemic was referred to by some as ‘the great equalizer’, something which would bring the world together in its effort to curb the effects of the virus. The slogan ‘no one is safe, until everyone is safe’ became well known and is still in use today.
However, it quickly became apparent that even though we were all weathering the same storm, not everyone was in the same boat. Some boats were well insulated and packed with essentials which equipped their passengers to carry on indefinitely. But others were filling with water from all sides, completely caught off guard in terms of supplies, leaving those onboard desperate for outside intervention. Furthermore, even those individuals who found themselves on the same boat, quickly realized that they had different roles to play. The women on the boats had to look after the children, cook what little food they had and still manage to assist in keeping the boat from sinking.
Of course this is an analogy for the higher and lower income countries of the world but it can apply as pertinently within developing nations, such as those in Africa where the top 10% of income earners receive half of the all household income.[1]
Global vaccine distribution
More than a year and a half into the pandemic and for some developing countries, the end to COVID-19 seems further away than it seemed at the start.
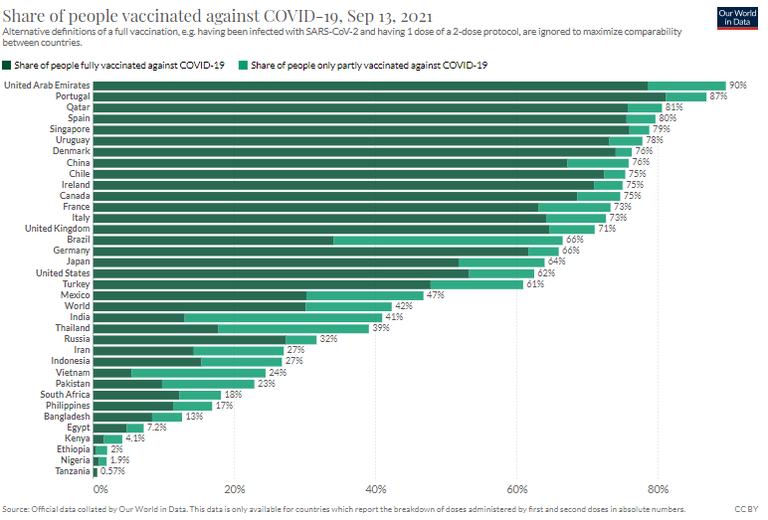
According to the Oxford Martin School at the University of Oxford, on 23 August 2021
‘42.3% of the world population has received at least one dose of a COVID-19 vaccine. 5.76 billion doses have been administered globally, and 33 million are now administered each day. Only 1.9% of people in low income countries have received at least one dose.’[2]
Disparities between countries are demonstrated in the figure below.
High income countries have been able to source their vaccines through bilateral agreements directly with vaccine manufacturers, while low income countries have had to rely largely on mechanisms such as the Covid-19 Vaccine Global Access facility (COVAX facility).
Countries with a large amount of bargaining power have secured doses, often in excess of need, of the most effective vaccines at prices which are unknown to the rest of the world. African countries, with little or no bargaining power, have had to wait for their turn in the vaccine distribution queue, ultimately getting whatever vaccine was left.
COVAX: Africa’s hope or disappointment?
As has been explored in a previous brief, the COVAX facility was established to create a ‘pooled procurement mechanism to secure adequate and equitable supplies of vaccines at competitive prices for countries throughout the world, irrespective of their wealth status’.[3] However, as of 30 July 2021, the COVAX facility had only supplied ‘about 3.8% of total inoculations’ worldwide, citing reasons such as underfunding and vaccine hoarding for their ineffectiveness.[4] Moreover, some of these vaccines have gone to high income countries which had already secured enough vaccines through bilateral deals to vaccinate their entire populations, instead of allocating all of them to low income countries, and particularly to Africa, which has not yet managed to vaccinate all health care workers and priority groups.
Although vaccine hoarding and funding have been obstacles resulting in a lack of supply for the COVAX facility, COVAX itself has ‘ultimately led to the entrenchment of unequal global vaccine access’.[5] This is because self-financing countries can participate in COVAX through a Committed Purchase or an Optional Purchase Agreement. On the other hand, the COVAX Advance Market Commitment, funded mainly through official development assistance and contributions from the private sector and philanthropy, will enable access to COVID-19 vaccines for lower-income economies.
Under an Optional Purchase Agreement countries can choose to opt out of receiving any particular vaccine, without jeopardising their ability to receive their full share of doses of other vaccines.
‘Participants could choose to pick their vaccine of choice subject to supply availability. Therefore, depending on efficacy levels, self-financing countries could access vaccines based on preference, leaving low income countries with no choice but to take what is left over. This type of agreement may be more attractive to participants that already have bilateral agreements with manufacturers, through which they may already have secured sufficient doses of that particular vaccine.’[6]
The current structure of COVAX vaccine procurement and distribution thus fail to ensure that people in all corners of the world will get equal access to COVID-19 vaccines once they are available, regardless of their wealth’.
The manner in which COVAX engages with both vaccine suppliers and recipient countries has also proven detrimental to equal and fair vaccine access through the negotiation process. Negotiations and contracts have been characterised by secrecy and a lack of transparency in general. The COVAX deals are no exception. The COVAX facility has claimed that ‘confidentiality serves the goals of getting good deals’. But by keeping the negotiations secret, COVAX obscures the extent to which high income countries benefit by ‘double dipping’ into the vaccine pool.[7]
Conclusion
Accountability requires transparency. Without the required facts, it is impossible to hold those in charge accountable for the failed attempt at ensuring equal access to vaccines for all nations. Low income countries are at the mercy of the COVAX facility and high income countries with surplus supplies of vaccines, to the extent that they are unable to engage in deals with manufacturers. The widening gap between high and low income countries in terms of both vaccine procurement and distribution is a massive problem. It means that people in low income countries will be subject to severe non-pharmaceutical restrictions, such as lockdowns and travel bans, for a long time.
While COVAX deliveries and donations trickle into these lower income countries, there are other issues such as logistics and roll out plans which also need to be taken into consideration. These issues, particularly on the African continent, and their impact will be considered in the second brief.
Sophie Smit
Legal Researcher
sophie@hsf.org.za
[3]Republic of South Africa: Department of Health ‘Covid-19 online resource and news portal’, available here.
[4] Suhail Omar ‘COVAX isn't Africa's silver bullet’ Democracy and society (30 July 2021), available here.